Harvey J. Alter, Michael Houghton and Charles M. Rice share the award for identifying the virus behind the blood-borne liver disease
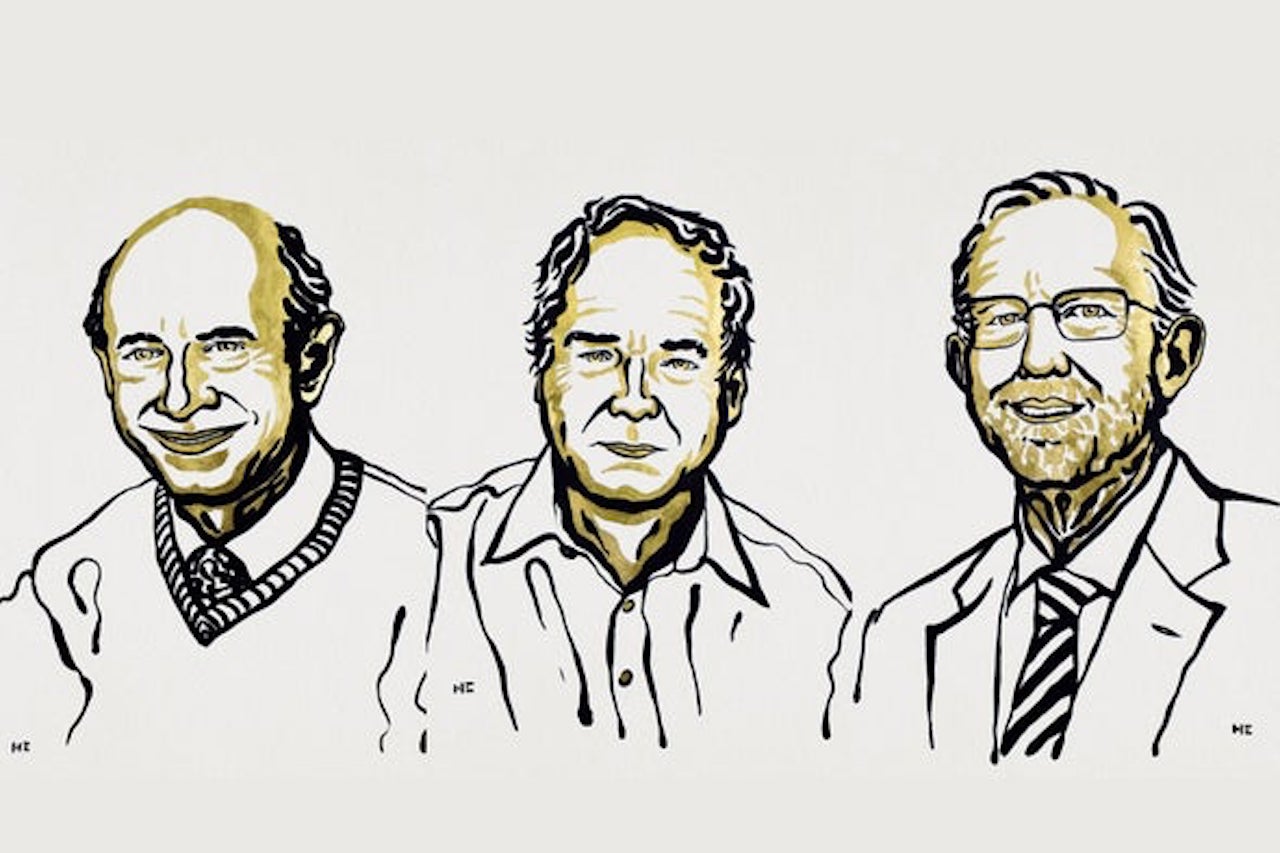
This year’s Nobel Prize in Physiology or Medicine was awarded for the discovery of the hepatitis C virus, which causes severe liver disease and chronically infects more than 70 million people worldwide. The prize was jointly awarded to American researchers Harvey J. Alter and Charles M. Rice and British-born scientist Michael Houghton.
Three hepatitis viruses are known to infect the liver: Hepatitis A is transmitted by water or contaminated food, and it causes a short-term infection that is typically resolved within weeks. Hepatitis B and C are transmitted by contaminated blood, and they cause chronic infections that can silently attack the liver for decades. This damage can lead to cirrhosis or liver cancer, which are sometimes only treatable through liver transplants. As a result of hepatitis C’s discovery and blood-screening programs, the virus has been nearly eliminated, and most cases are treatable.
“I’m surprised but not that surprised” about the Nobel announcement, says Timothy Sheahan, a virologist and an assistant professor of epidemiology at the University of North Carolina at Chapel Hill’s Gillings School of Public Health. Sheahan did his postdoctoral work on hepatitis C in Rice’s laboratory at the Rockefeller University. “Charlie Rice’s work in discovering the hepatitis C virus and creating systems to study the biology and do drug discovery for [the virus] led to the development of antiviral drugs that can cure people of hepatitis C. The same effort … led to the discovery and use of what is now called remdesivir,” an antiviral drug that has been shown to shorten the duration of COVID-19, adds Sheahan, who has studied the medication’s effectiveness against SARS-CoV-2 and other coronaviruses. “And now this is being used on the president of the United States.”
Hepatitis B and C were first noticed in patients who had received numerous blood transfusions or therapeutics made from donated blood. In the mid-1960s American physician Baruch Blumberg discovered the hepatitis B virus (for which he was awarded the 1976 Nobel Prize in Physiology or Medicine). But this virus did not explain all cases of post-transfusion liver disease. In the late 1960s, Alter, who was then working at the National Institutes of Health Blood Bank, began to suspect an as yet unknown pathogen was causing the disease. He later showed that the illness could be transferred to monkeys from patients’ blood.
Isolating the hepatitis C virus was harder, but Houghton—then working at the pharmaceutical company Chiron—and his colleagues were able to successfully clone it in 1989 by introducing viral DNA from an infected animal into bacteria, and using human antibodies to the virus to screen for its genetic sequence. They found that Hepatitis C resembled viruses from a family called flaviviruses. It was the first time this type of molecular biology approach had been used to identify a virus. The discovery led to a blood test that could screen for hepatitis C. This immediately reduced the number of cases resulting from blood transfusions worldwide.
But one question remained: Did the virus alone cause disease? Rice, then at Washington University in St. Louis, and his colleagues cloned the pathogen and injected the copies into animals, but the virus did not replicate. When Rice compared the sequences of many viral clones, he saw they contained genetic mutations that made them defective. But when he repaired the mutations, the clones caused clinical signs of hepatitis C in chimpanzees. This result showed that the cloned virus could cause disease.
“I think Alter truly deserved it,” says Patrizia Farci, chief of the hepatic pathogenesis section at the National Institute of Allergy and Infectious Diseases, who has been collaborating with him for years. “This work, together with [that of] Michael Houghton and Charlie Rice, has saved millions of lives and also shows that science does not have any barrier.” Farci first met Alter in the 1980s, and she says he used to write and read poetry about science. “He’s not only science!” she adds.
Sheahan speaks similarly highly of Rice. “He’s just a special person,” Sheahan says. “I’ve had two mentors, [including Rice]. They’re both really smart. But these are famous people who are actually good at being humans.”
“All three laureates have made tremendous contributions,” says Angela Rasmussen, a virologist and an associate research scientist at the Columbia University Mailman School of Public Health. Rasmussen, who did her postdoctoral work on the hepatitis C virus (but not with Alter, Houghton or Rice). She admits she was a bit surprised that the award went to this area of research. though shesays it is very relevant because hepatitis C is itself a pandemic. While Rasmussen says the recipients are all deserving, she notes that the Nobel Committee has once again honored three white men with the prestigious award. “It really puzzles me that the Nobel Committee says they are awarding the best science,” she says, “but the reality is: there are lots of people contributing to the best science that are women and people of color. They could do more to address that disparity.”
Last year’s prize was awarded to scientists William Kaelin, Jr., Peter Ratcliffe and Gregg Semenza for the discovery of how cells sense oxygen.



